Well-Woman Chart
Recommendations for Well-Woman Care
Preventive care visits provide an excellent opportunity for well-woman care including screening, evaluation of health risks and needs, counseling, and immunizations. Recommendations for Well-Woman Care – A Well-Woman Chart was developed by the Women’s Preventive Services Initiative (WPSI). The Well-Woman Chart outlines preventive services recommended by the WPSI, U.S. Preventive Services Task Force (USPSTF), and Bright Futures based on age, health status, and risk factors. Additional recommendations for immunizations are provided in a separate table from the Advisory Committee on Immunization Practices. Clinical practice considerations, risk assessment methods, and the age and frequency to deliver services are described in the Clinical Summary Tables that accompany the chart.
The Recommendations for Well-Woman Care – A Well-Woman Chart provides a framework for incorporating preventive health services for women into clinical practice. These services may be completed at a single visit or as part of a series of visits that take place over time. Recommendations from the WPSI and the USPSTF for preventive services for pregnant and postpartum women are also provided in the Well-Woman Chart. Comprehensive recommendations for pregnant and postpartum women can be found in ACOG’s practice guidelines and other educational materials. The recommendations are not intended as a statement of the standard of care and do not comprise all proper treatments or methods of care. Providers should use clinical judgment in applying these recommendations to individual patient care, taking into account the needs and resources particular to the locality, the institution, or the type of practice. The Chart is updated annually.
The updated Spanish version will be available soon.

In addition to the printable PDF file, an interactive Well-Woman Chart can be accessed below.
Interactive Well-Woman Chart
Prevention Services
GENERAL HEALTH
INFECTIOUS DISEASES
CANCER
Prevention services for pregnancy and postpartum provided in addition to age-based services listed above.
PREGNANCY
| PREGNANCY | |
|---|---|
| Anxiety screening | |
| Bacteriuria screening | |
| Breastfeeding counseling, services & supplies | |
| Contraception & contraceptive care | |
| Depression screening & preventive interventions 21 | |
| Diabetes Screening 22 | |
| Folic acid supplementation | |
| Gonorrhea & chlamydia screening | |
| Healthy weight gain counseling | |
| Hepatitis B screening | |
| HIV testing (each pregnancy) | |
| Interpersonal & domestic violence screening | |
| Preeclampsia prevention with low-dose aspirin 23 | |
| Preeclampsia screening | |
| Rh(D) blood typing | |
| Substance use screening & assessment | |
| Syphilis screening | |
| Tobacco screening & counseling |
POSTPARTUM
| POSTPARTUM | |
|---|---|
| Anxiety screening | |
| Breastfeeding counseling, services & supplies | |
| Contraception & contraceptive care | |
| Depression screening & preventative interventions21 | |
| Diabetes Screening 24 | |
| Folic acid supplementation | |
| Interpersonal & domestic violence screening | |
| Substance use screening & assessment | |
| Tobacco screening & counseling |
KEY:
Recommended by the USPSTF (A or B rating), WPSI, or Bright Futures
Recommended for selected groups
1 Additional Bright Futures recommendations include: Periodic vision and hearing tests ages 13 to 21; screening for suicide risk ages 13 to 21; risk assessment for sudden cardiac arrest and sudden cardiac death ages 13 to 21; risk assessment for anemia ages 13 to 21; and fluoride supplementation if needed ages 13 to 16.
Abbreviations:
- BRCA = breast cancer susceptibility gene;
- CVD = cardiovascular disease;
- HIV = human immunodeficiency virus;
- HCV = hepatitis C virus;
- HBV = hepatitis B virus;
- STI = sexually transmitted infection;
- USPSTF = U.S. Preventive Services Task Force;
- WPSI = Women’s Preventive Services Initiative.
*Criteria for Selective Screening
- Diabetes screening: Screen women with overweight or obese BMI ages 35 to 70 years; and women with previous gestational diabetes but not previously diagnosed with type 2 diabetes when not pregnant ages ≥13 years.
- Folic acid supplementation: Sexually active and planning or capable of pregnancy.
- Healthy diet and physical activity counseling: Overweight or obese BMI and additional CVD risk factors (hypertension, dyslipidemia, abnormal blood glucose levels, diabetes).
- Lipid screening: Lipid testing is needed to calculate 10-year CVD risk in adults. Screen adolescents ages 13 to 17 years with familial dyslipidemia, risk factors, or high-risk conditions.
- Osteoporosis screening: 10-year fracture risk equivalent to an average-risk 65-year-old woman based on specific risk factors (parental history of hip fracture, smoking, excess alcohol consumption, low body weight).
- Statin use to prevent CVD: Ages 40 to 75 years, one or more CVD risk factors (i.e., dyslipidemia, diabetes, hypertension, or smoking), and calculated 10-year risk of a CVD event ≥10%.
- Urinary incontinence screening: Screen all women ages ≥18 and younger women if postpartum.
- Chlamydia and gonorrhea screening: New sex partner, more than one sex partner, a sex partner with concurrent partners, or a sex partner who has an STI; inconsistent condom use among persons who are not in mutually monogamous relationships; previous or coexisting STI; and exchanging sex for money or drugs. Prevalence is also higher among incarcerated populations, military recruits, and patients receiving care at public STI clinics.
- Hepatitis B screening: Born in a country with a prevalence of HBV infection ≥2%; lack of vaccination in infancy in U.S.-born persons with parents from a country or region with prevalence ≥8%; HIV-positive; injection drug use; and household contacts or sexual partners of persons with HBV infection.
- Hepatitis C screening: One-time screening for asymptomatic adults ages 18 to 79 without known liver disease. Repeat screening and screen at other ages if past or current injection drug use.
- HIV preexposure prophylaxis (PrEP): Candidates include 1) heterosexually active women with a sexual partner who has HIV; or inconsistent or no use of condoms during sex with a partner whose HIV status is unknown and who is at high risk; or an STI with syphilis or gonorrhea within the past 6 months; 2) uses injection drugs and shared use of drug injection equipment; or has a drug-injecting partner who has HIV; 3) engaged in transactional sex, such as for money, drugs, or other.
- Immunizations should be administered according to the most recent Advisory Committee on Immunization Practices (ACIP) recommendations. Accessed December 11, 2023.
- Sexually transmitted infection prevention counseling: Risk factors for STIs include having an STI currently or within the past year, not consistently using condoms, having multiple sex partners, or having sex partners within populations with a high prevalence of STIs. Increased STI prevalence rates are found among women seeking STI testing or attending STI clinics; sexual and gender minorities; and among those with HIV, using injection drugs, exchanging sex for money or drugs, or residing in correctional facilities.
- Syphilis screening: Women with HIV; high prevalence communities or populations; history of incarceration; exchanging sex for money or drugs.
- Tuberculosis infection: Persons from countries with increased tuberculosis prevalence; living in high-risk congregate settings (e.g., homeless shelters, correctional facilities); exposure to individuals with active tuberculosis, such as health care workers and workers in high-risk congregate settings; immunosuppressed individuals; patients with silicosis.
- Breast cancer screening: Decisions about screening are made on an individual basis according to risk and preferences through a shared-decision making process.
- Lung cancer screening: 20 pack-year smoking history and currently smoke or have quit within the past 15 years.
- Medications to reduce breast cancer risk: Risk factors for breast cancer include increasing age, family history of breast or ovarian cancer (especially among first-degree relatives and onset before age 50 years), history of atypical hyperplasia or other nonmalignant high-risk breast lesions, previous breast biopsy, and extremely dense breast tissue. Models suggest that women with an estimated 5-year breast cancer risk of 3% or greater are likely to have more benefit than harm, although the balance of benefits and harms depends on age, the medication used, and whether the patient has a uterus.
- Skin cancer counseling: Fair skin, light hair and eye color, freckles, sunburn easily.
- Perinatal depression preventive interventions: Counseling interventions for women with one or more of the following: a history of depression, current depressive symptoms that may not reach a diagnostic threshold, socioeconomic risk factors such as low income or adolescent or single parenthood, recent intimate partner violence, or mental health–related factors such as elevated anxiety symptoms or a history of significant negative life events.
- Diabetes screening during pregnancy: Universal screening after 24 weeks’ gestation (preferably 24 to 28 weeks); additionally, selective screening if risk factors before 24 weeks’ gestation, ideally at the first prenatal visit (obese BMI; older maternal age; history of gestational diabetes; family history of diabetes; ancestry with increased risk for type 2 diabetes [Hispanic, Native American, South or East Asian, African American, or Pacific Islands descent]).
- Preeclampsia prevention with low-dose aspirin: History of preeclampsia, especially when accompanied by an adverse outcome; multifetal gestation; chronic hypertension; type 1 or 2 diabetes; renal disease; autoimmune disease (systemic lupus erythematous, antiphospholipid syndrome).
- Diabetes screening after pregnancy: Previous gestational diabetes but not previously diagnosed with type 2 diabetes when not pregnant ages ≥13 years.
Suggested Citation
Women’s Preventive Services Initiative. Recommendations for well-woman care – a well-woman chart. Washington, DC: ACOG Foundation; 2024. Available at: https://www.womenspreventivehealth.org/wp-content/uploads/FINAL_2024-Well-Woman-Chart-English.pdf . Retrieved January 30, 2024.
Women’s Preventive Services Initiative. Recommendations for well-woman care: clinical summary tables. Washington, DC: ACOG Foundation; 2024. Available at: https://www.womenspreventivehealth.org/wp-content/uploads/FINAL-WPSI-Clinical-Summary-Tables-2024.pdf. Retrieved January 30, 2024.
Inquiries
All inquiries regarding HRSA acceptance and support of the WPSI recommendations should be sent to wellwomancare@hrsa.gov. Inquiries regarding the content or evidence related to the recommendations can be sent to wpsi@acog.org.
©2024, Content owned by the ACOG Foundation, all Marks and Rights Reserved. This project was supported by the Health Resources and Services Administration (HRSA) of the U.S. Department of Health and Human Services (HHS) under grant number UHOMC29940, Bright Futures for Women’s Health: Standard Practice Guidelines for Well Women Care. This information or content and conclusions are those of the author and should not be construed as the official position nor policy of, nor should any endorsements be inferred by HRSA, HHS, or the U.S. Government.
How to Get the Well-Woman Chart Shortcut on Your Smartphone
The Women’s Preventive Services Initiative’s (WPSI) Recommendations for Well-Woman Care – A Well-Woman Chart summarizes preventive service recommendations for women from the WPSI, U.S. Preventive Services Task Force (USPSTF) and Bright Futures. The Well-Woman Chart provides a framework for incorporating preventive health services for women into clinical practice. To increase accessibility of these recommendations, the digitally-interactive version of the Well-Woman Chart can be added as a shortcut to your mobile device. Please note an internet connection is required to access the Well-Woman Chart from the home screen shortcut.
Follow these step-by-step instructions to add the Well-Woman Chart shortcut to the home screen of your mobile device.
Well-Woman Chart Shortcut for iPhone
- Visit www.acog.org/WellWomanChart from your mobile device.
- Tap the Options icon towards the bottom of the screen.
- Tap the “Add to Home Screen” star icon.
- Edit the shortcut name to “WPSI.”
- See the shortcut appear.
Well-Woman Chart Shortcut for Android
- Visit www.acog.org/WellWomanChart from your mobile device.
- Tap the Menu icon towards the top, right of the screen.
- Tap the “Add to Home Screen” icon.
- Edit the shortcut name to “WPSI.”
- See the shortcut appear.
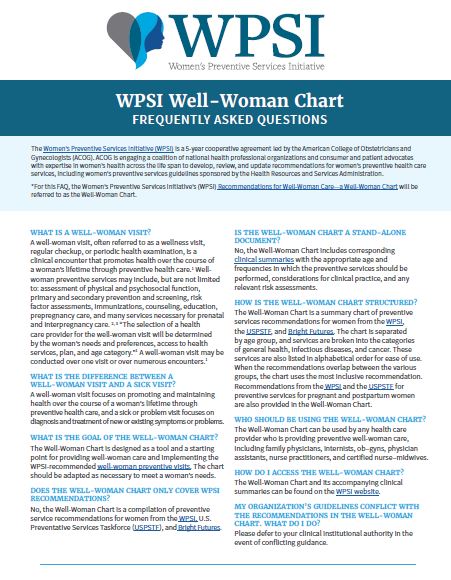
Frequently Asked Questions
Recommendations for Well-Woman Care – A Well-Woman Chart is a resource developed by the Women’s Preventive Services Initiative (WPSI) that summarizes age-based preventive service recommendations for women from adolescence into maturity. Scroll down for frequently asked questions and answers about the chart.
*For this FAQ, the Women’s Preventive Services Initiative’s (WPSI) Recommendations for Well-Woman Care—a Well-Woman Chart will be referred to as the Well-Woman Chart.
Download the PDF version below.
What is a Well-Woman Visit?
A well-woman visit, often referred to as a wellness visit, regular checkup, or periodic health examination, is a clinical encounter that promotes health over the course of a woman’s lifetime through preventive health care1. Well-woman preventive services may include, but are not limited to: assessment of physical and psychosocial function, primary and secondary prevention and screening, risk factor assessments, immunizations, counseling, education, prepregnancy care, and many services necessary for prenatal and interpregnancy care2,3. “The selection of a health care provider for the well-woman visit will be determined by the woman’s needs and preferences, access to health services, plan, and age category.”1 A well-woman visit may be conducted over one visit or over numerous encounters1.
What is the difference between a well-woman visit and a sick visit?
A well-woman visit focuses on promoting and maintaining health over the course of a woman’s lifetime through preventive health care, and a sick or problem visit focuses on diagnosis and treatment of new or existing symptoms or problems.
What is the goal of the well-woman chart?
The Well-Woman Chart is designed as a tool and a starting point for providing well-woman care and implementing the WPSI-recommended well-woman preventive visits. The chart should be adapted as necessary to meet a woman’s needs.
Does the well-woman chart only cover WPSI recommendations?
Does the well-woman chart only cover WPSI recommendations?
No, the Well-Woman Chart is a compilation of preventive service recommendations for women from the WPSI, U.S. Preventative Services Taskforce (USPSTF), and Bright Futures.
Is the well-woman chart a stand-alone document?
No, the Well-Woman Chart includes corresponding clinical summaries with the appropriate age and frequencies in which the preventive services should be performed, considerations for clinical practice, and any relevant risk assessments.
How is the well-woman chart structured?
The Well-Woman Chart is a summary chart of preventive services recommendations for women from the WPSI, the USPSTF, and Bright Futures. The chart is separated by age group, and services are broken into the categories of general health, infectious diseases, and cancer. These services are also listed in alphabetical order for ease of use. When the recommendations overlap between the various groups, the chart uses the most inclusive recommendation. Recommendations from the WPSI and the USPSTF for preventive services for pregnant and postpartum women are also provided in the Well-Woman Chart.
Who should be using the well-woman chart?
The Well-Woman Chart can be used by any health care provider who is providing preventive well-woman care, including family physicians, internists, ob–gyns, physician assistants, nurse practitioners, and certified nurse–midwives.
How do I access the well-woman chart?
The Well-Woman Chart and its accompanying clinical summaries can be found on the WPSI website.
My organization's guidelines conflict with the recommendations in the well-woman chart. What do I do?
Please defer to your clinical institutional authority in the event of conflicting guidance.
Do women need a well-woman visit every year?
The WPSI recommends that women receive at least one preventive care visit per year beginning in adolescence and continuing across the life span to ensure that the recommended preventive services are obtained.
How do I prioritize well-woman exam services in the time allotted for each woman?
Each woman is unique, as are her health care needs. Decisions regarding when to initiate screening, how often to screen, and when to stop screening should be based on a periodic shared decision-making process involving the woman and her health care provider. The shared decision-making process assists women in making an informed decision and includes, but is not limited to, a discussion about the benefits and harms of screening; an assessment of the woman’s values and preferences; and consideration of factors such as life expectancy, comorbidities, and health status.2
Do I need to do all these services in one visit?
The services listed in the Well-Woman Chart should not be viewed as what is expected to be performed at every well-woman visit by every health care provider. Additional well-woman visits may be needed to obtain all necessary services depending on a woman’s age, health status, reproductive health needs, pregnancy status, and risk factors.
What about health insurance coverage?
All recommendations listed on the Well-Woman Chart include clinical preventive services that most private insurance plans and many Medicaid state programs cover without cost-sharing as required by the Affordable Care Act. For more information about federal coverage requirements for preventive services, refer to healthcare.gov and your insurance carrier.
Do you have any resources to assist with billing?
The American College of Obstetricians and Gynecologists (ACOG) offers coding resources. You can also submit coding questions to the ACOG coding team through our Coding Ticket Database. This resource is available to both ACOG members and nonmembers.
What about immunizations?
Immunizations should be administered according to the most recent ACIP recommendations.
References
- Conry, Brown. Well-Woman Task Force: Components of the Well-Woman Visit. Obstetrics & Gynecology 2015; 126: 697-701. https://journals.lww.com/greenjournal/Fulltext/2015/10000/Well_Woman_Task_Force__Components_of_the.2.aspx
- Women’s Preventive Services Initiative. Recommendations for preventive services for women: final report to the U.S. Department of Health and Human Services, Health Resources and Services Administration. Washington, D.C.: American College of Obstetricians and Gynecologists; 2016.
- Well-woman visit. ACOG Committee Opinion No. 755. American College of Obstetricians and Gynecologists. Obstetrics & Gynecology 2018; 132: 181–86. https://journals.lww.com/greenjournal/Fulltext/2018/10000/ACOG_Committee_Opinion_No__755_Summary__.57.aspx
- U.S. Department of Health and Human Resources Women’s Preventive Services Guidelines. https://www.hrsa.gov/womens-guidelines-2016/index.html – Accessed August 15, 2018.